All-On-X Dental Implants: A Fixed Solution for Replacing Many Teeth at Once
When most or all teeth are missing—or when teeth are failing—people often want one clear answer: “What can help me eat comfortably again and stop worrying about loose teeth?” That question matters because it’s not only about appearance. It’s about function, comfort, and the freedom to live your day without planning around your mouth. All-on-X treatment is designed for that exact situation: replacing a full arch of teeth with a stable, fixed set that stays in place.
This article explains how All-on-X treatment works, what the journey looks like, and why many patients choose this approach when they’re ready for a bigger change.
What All-On-X Dental Implants Mean and Why “X” Matters
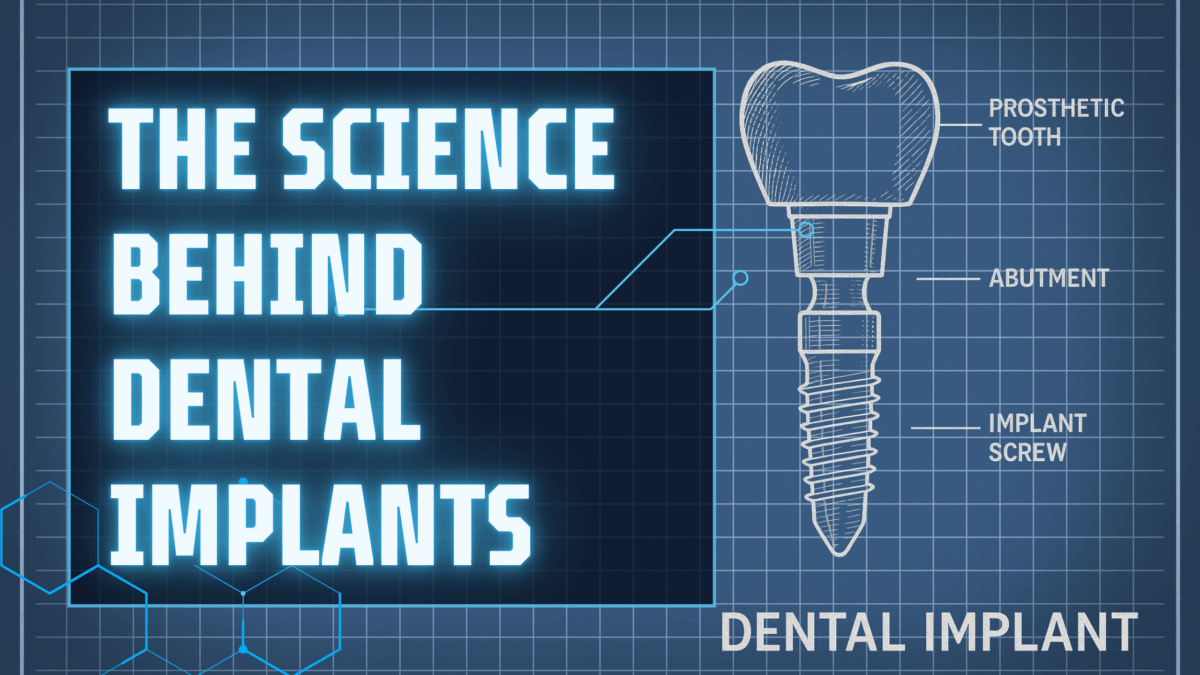
All-on-X treatment describes a full-arch replacement supported by a specific number of implants. The “X” simply stands for the number of implants used to support the new arch. Some plans may use four implants, others may use five or six, depending on bone support, bite forces, and your anatomy.
The big idea is this: instead of placing one implant for every missing tooth, All-On-X Dental Implants use a strategic set of implants to hold a full row of teeth. Those teeth are connected in one piece, so the bite force is shared across the implants. This can be a practical way to rebuild a full smile with fewer implants than a “one tooth at a time” approach.
Patients often like that All-On-X Dental Implants are fixed in place. That means the teeth do not come out at night, and you don’t have to rely on adhesives. You clean them daily like teeth, but they stay put.
Who Typically Considers All-On-X Dental Implants?
People explore All-On-X Dental Implants for several common reasons:
- They are missing many teeth in the upper or lower jaw
- Their current denture feels loose or rubs sore spots
- They have teeth that are breaking down from decay or gum disease
- They want a fixed option instead of something removable
- They want a plan that can improve chewing comfort and day-to-day confidence
An evaluation is still essential. During planning for All-On-X Dental Implants, your dental team looks at bone levels, gum health, the shape of your jaw, and your bite. They also review health history because healing matters for long-term success.
If there are active infections or gum issues, those are treated first. If bone is thin in certain areas, planning may include grafting or adjusting implant positions. The goal is to place implants where they can be supported well, then build an arch that fits your face and your bite.
What the All-On-X Dental Implants Process Can Look Like
Every plan is customized, but many patients find the process easier once they understand the steps. Here’s a patient-friendly overview of what All-On-X Dental Implants may involve.
Step 1: Consultation and imaging
This is the “map-making” stage. Imaging helps the team see bone levels, sinus spaces, and nerve pathways. Careful planning is a major reason All-On-X Dental Implants can be predictable and safe.
Step 2: Creating a step-by-step plan
Your plan may include removing failing teeth, treating gum infection, and choosing implant positions. The team also talks through what type of temporary teeth you may wear while healing. With All-On-X Dental Implants, temporary teeth can be an important part of the journey because they support function and comfort during the transition.
Step 3: Surgery day and comfort options
On the day of surgery, the dental team prepares the mouth and places the implants. Many patients choose calming options, and some plans include Sedation Dentistry for a smoother experience. You’ll also receive clear instructions for home care and eating while the area heals.
Step 4: Healing and strengthening
Over the next few months, the bone bonds around the implants. This is the foundation stage for All-On-X Dental Implants. During this time, a temporary set of teeth may be adjusted as your gums settle.
Step 5: Final teeth designed for long-term function
Once healing is complete, the final arch is created. The goal is not just a bright smile, but a strong bite that fits your jaw and protects the implants. With All-On-X Dental Implants, the final prosthetic is designed to balance comfort, durability, and a natural look.
Everyday Life with All-On-X Dental Implants: Eating, Speaking, and Cleaning
One reason patients choose All-On-X Dental Implants is the day-to-day experience. A fixed arch often feels more stable than a removable denture, which can reduce worry about shifting during meals or conversations.
Eating
After healing, many people feel they can enjoy a wider range of foods. You still want to be smart—hard ice and using teeth as tools are never great ideas—but the goal with All-On-X Dental Implants is comfortable, reliable chewing.
Speaking
A stable arch can make speech feel more natural, especially for patients who struggled with a loose denture. Your mouth may need a short “adjustment period” as your tongue and cheeks get used to the new shape, but most patients adapt well.
Cleaning
Cleaning is simple but important. You’ll brush twice daily and clean around the gumline and under the arch using tools your dental team recommends (like floss threaders, special brushes, or a water flosser). Routine professional visits are also important. Even though the teeth are not natural, the gums and bone still need healthy care for All-On-X Dental Implants to last.
Benefits of All-On-X Dental Implants Supported by Professional Guidance
Professional dental material often highlights that full-arch replacement should be planned with both function and long-term health in mind. All-On-X Dental Implants are frequently discussed as a reliable option because they focus on stability, controlled placement, and a fixed result.
Benefits commonly emphasized in professional guidance include:
- A fixed set of teeth: All-On-X Dental Implants stay in place, reducing the need for adhesives and nightly removal.
- Better stability than many removable options: Implant support can reduce movement and sore spots.
- A stronger chewing experience: Many patients report improved comfort and the ability to enjoy more foods.
- Support for jawbone function: Restoring chewing forces can help reduce ongoing bone changes linked to tooth loss.
- A single, coordinated plan: Instead of managing many separate tooth problems, All-On-X Dental Implants can address a full arch in one organized treatment pathway.
Professional guidance also stresses that success depends on proper planning, healthy gums, and ongoing maintenance. Regular checkups, cleanings, and good home care protect the tissues that support All-On-X Dental Implants.
Final Thoughts: Rebuilding an Entire Smile with Confidence
All-On-X Dental Implants can be a life-changing option for people who need a full-arch solution. They are designed to create a fixed, stable set of teeth that supports eating, speaking, and day-to-day comfort. The journey starts with a personalized evaluation, then moves through careful planning, healing, and a final restoration made to fit you.
Ready to explore whether All-On-X Dental Implants are a match for your goals? Contact Secure Dental to schedule your consultation and book an appointment at a location near you. Secure Dental has 9 offices across Iowa, Indiana, Illinois, and Tennessee to help you move forward with a stable, confident smile.